PREVALENCE AND MOLECULAR CHARACTERIZATION OF <i>BLA<sup>TEM</sup></i>, <i>BLA<sup>SHV</sup></i> AND <i>BLA<sup>CTX-M</sup></i><sup> </sup>GENES IN ESBL-PRODUCING <i>Escherichia coli</i> AND <i>Klebsiella pneumoniae</i> ISOLATED FROM INTENSIVE CARE UNIT PATIENTS
Abstract
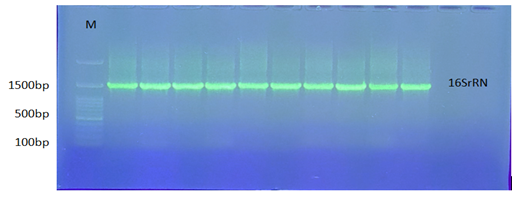
The rise and spread of antimicrobial resistance (AMR) not only significantly hinder the effective treatment of infectious diseases, but also lead to prolonged illness, treatment failures, and increased mortality. In intensive care units (ICUs), extended-spectrum β-lactamase (ESBL)-producing bacteria, such as Escherichia coli (E. coli) and Klebsiella pneumoniae (K. pneumoniae), are among the most concerning multidrug-resistant organisms (MDROs. This research was conducted to find out the causative agents of ICU infections, identify their profiles of antimicrobial resistance, and assess associated virulence factors. Discrepancies were found in bacterial identification by molecular analysis using 16S rRNA sequencing compared to the Vitek2 system. More than half (50%) carried all three ESBL genes, while the prevalence of blaSHV + blaCTX-M carriers were the lowest. Isolates of E. coli from the study were not found to be salmon single ESBL genes (blaSHV, blaCTX, or blaTEM), only 5.26% of K. pneumoniae isolates carried blaTEM among them. Most of the strains had moderate to high biofilm-forming ability, which is the key to their MDR. In other words, ICU patients are vulnerable to colonization and infection with MDR pathogens, and still, E. coli and K. pneumoniae are the major threats that are linked to the resistance mechanisms and virulence factors of these pathogens.
Full text article
References
Alameer, K. M., Abuageelah, B. M., Alharbi, R. H., Alfaifi, M. H., Hurissi, E., Haddad, M., Dhayhi, N., Jafar, A. S., Mobarki, M., Awashi, H., Musawi, S., Alameer, A. M., Kariri, S. H., & Alhazmi, A. H. (2025). Retrospective Analysis of Antibiotic Resistance Patterns of Uropathogenic Escherichia coli With ExtendedFocus on -Spectrum β-Lactamase at a Tertiary Central Hospital in Saudi Arabia. Health science reports, 8(1), e70378. https://doi.org/10.1002/hsr2.70378
Ali, B. N. (2025). Molecular Detection of Drug-Resistant Genes Among Clostridioides Difficile From Diarrheic Children In Duhok City -Iraq. Science Journal of University of Zakho, 13(2), 179–184. https://doi.org/10.25271/sjuoz.2025.13.2.1424
Al-Qaysi A, Ahmed M, Habeeb W, Al-Meani S, Janaby M, Alalwani A, Aljanaby S, Edan A, Alani S, Hammood M, Abaas M. (2024). Genetic Variants of Multidrug-Resistant Klebsiella pneumoniae Isolated from Al-Ramadi Teaching Hospital, Iraq. Open Microbiol J, 2024; 18: e18742858298979. http://dx.doi.org/10.2174/0118742858298979240628070603
Babypadmini, S., & Appalaraju, B. (2004). Extended spectrum-lactamases in urinary isolates of Escherichia coli and Klebsiella pneumoniae—Prevalence and susceptibility pattern in a tertiary care hospital. Indian Journal of Medical Microbiology, 22(3), 172–174. doi.org/10.1016/s0255-0857(21)02830-9
Balouiri, M., Sadiki, M., & Ibnsouda, S. K. (2016). Methods for in vitro evaluating antimicrobial activity: A review. Journal of pharmaceutical analysis, 6(2), 71–79. doi.org/10.1016/j.jpha.2015.11.005
Bonnet R. (2004). Growing group of extended-spectrum beta-lactamases: the CTX-M enzymes. Antimicrobial agents and chemotherapy, 48(1), 1–14. doi.org/10.1128/AAC.48.1.1-14.2004
Bosshard, P., Abels, S., Zbinden, R., Böttger, E., & Altwegg, M. (2003). Ribosomal DNA sequencing for identification of aerobic gram-positive rods in the clinical laboratory: An 18-month evaluation. Journal of Clinical Microbiology, 41(9), 4134–4140. doi.org/10.1128/jcm.41.9.4134-4140.2003
Bradford, P. A. (2001). Extended-spectrum β-lactamases in the 21st century: Characterization, epidemiology, and detection of this important resistance threat. Clinical Microbiology Reviews, 14(4), 933–951. doi.org/10.1128/cmr.14.4.933-951.2001
Bush, K., & Bradford, P. A. (2016). β-Lactams and β-Lactamase Inhibitors: An Overview. Cold Spring Harbor perspectives in medicine, 6(8), a025247. doi.org/10.1101/cshperspect.a025247
Castanheira, M., Simner, P. J., & Bradford, P. A. (2021). Extended-spectrum β-lactamases: an update on their characteristics, epidemiology and detection. JAC-antimicrobial resistance, 3(3), dlab092. https://doi.org/10.1093/jacamr/dlab092
Chowdhury, S., & Parial, R. (2015). Antibiotic susceptibility patterns of bacteria among urinary tract infection patients in Chittagong, Bangladesh. SMU Medical Journal, 2(1), 114–127. doi.org/10.3329/bjmm.v2i2.28842
Clarridge, J. E. (2004). Impact of 16S rRNA gene sequence analysis for identification of bacteria on clinical microbiology and infectious diseases. Clinical Microbiology Reviews, 17(4), 840–862. doi.org/10.1128/cmr.17.4.840-862.2004
Deka, N. (2014). Comparison of tissue culture plate method, tube method and Congo red agar method for the detection of biofilm formation by coagulase-negative Staphylococcus isolated from non-clinical isolates. International Journal of Current Microbiology and Applied Sciences, 3(10), 810–815. doi.org/10.7860/jcdr/2018/34795.11827
Delétoile, A., Decré, D., Courant, S., Passet, V., Audo, J., Grimont, P., Arlet, G., & Brisse, S. (2009). Phylogeny and identification of Pantoea species and typing of Pantoea agglomerans strains by multilocus gene sequencing. Journal of Clinical Microbiology, 47(2), 300–310. doi.org/10.1128/jcm.01916-08
Drancourt, M., Bollet, C., Carlioz, A., Martelin, R., Gayral, J.-P., & Raoult, D. (2000). 16S ribosomal DNA sequence analysis of a large collection of environmental and clinical unidentifiable bacterial isolates. Journal of Clinical Microbiology, 38(10), 3623–3630. doi.org/10.1128/jcm.38.10.3623-3630.2000
Ghenea, A. E., Zlatian, O. M., Cristea, O. M., Ungureanu, A., Mititelu, R. R., Balasoiu, A. T., Vasile, C. M., Salan, A. I., Iliuta, D., Popescu, M., & Udriștoiu, A. L. (2022). TEM, CTX-M, SHV genes in ESBL-producing Escherichia coli and Klebsiella pneumoniae isolated from clinical samples in a county clinical emergency hospital, Romania—Predominance of CTX-M-15. Antibiotics, 11(4), 503. doi.org/10.3390/antibiotics11040503
Gupta, S., Maheshwari, V., & Shah, R. (2017). Prevalence of ESBL-producing Escherichia coli and Klebsiella species among clinical isolates and their in vitro antimicrobial susceptibility pattern in a tertiary care hospital. International Journal of Current Microbiology and Applied Science, 6, 2295–2303. doi.org/10.20546/ijcmas.2017.610.272
Gurung, J., Khyriem, A. B., Banik, A., Lyngdoh, W. V., Choudhury, B., & Bhattacharyya, P. (2013). Association of biofilm production with multidrug resistance among clinical isolates of Acinetobacter baumannii and Pseudomonas aeruginosa from intensive care units. Indian Journal of Critical Care Medicine, 17(4), 214–218. doi.org/10.4103/0972-5229.118416
Hami, Iman A., and Khalid S. Ibrahim. (2023): "Incidence of methicillin-resistant Staphylococcus aureus (MRSA) recovered from patients with urinary tract infections in Zakho City/ Kurdistan-Iraq." Science Journal of University of Zakho 11.1: 91-97. https://DOI.org/10.25271/sjuoz.2023.11.1.1041
Høiby, N., Bjarnsholt, T., Givskov, M., Molin, S., & Ciofu, O. (2010). Antibiotic resistance of bacterial biofilms. International Journal of Antimicrobial Agents, 35, 322–332. doi.org/10.1007/978-1-4419-6084-9_10
Husna, A., Rahman, M. M., Badruzzaman, A. T. M., Sikder, M. H., Islam, M. R., Rahman, M. T., Alam, J., & Ashour, H. M. (2023). Extended-Spectrum β-Lactamases (ESBL): Challenges and Opportunities. Biomedicines, 11(11), 2937. https://doi.org/10.3390/biomedicines11112937
Hussein, N. H., Abdu-Allah, S. N., Taha, B. M., & Hussein, J. D. (2018). Biofilm formation of KPC-producing and non-KPC-producing Klebsiella pneumoniae ssp. pneumoniae and inhibitory effect of some watery plant extracts on biofilm formation. Journal of University of Babylon for Pure and Applied Sciences, 26, 66–76. doi.org/10.1093/jac/dkt487
Ibrahim, A. S., & Youssef, N. (2015). Prevalence of CTX-M, TEM and SHV beta-lactamases in clinical isolates of Escherichia coli and Klebsiella pneumoniae isolated from Aleppo University Hospitals, Aleppo, Syria. Archives of Clinical Infectious Diseases, 10(2). doi.org/10.5812/archcid.22540
Ibrahim D. R. (2023). Prevalence of Plasmid Mediated QNRA, QNRB and QNRS Among Clinical Escherichia Coli Isolated from Urinary Tract Infections in Duhok, Kurdistan Region of Iraq. Science Journal of University of Zakho. 11(4):523-31. https://DOI.org/10.25271/sjuoz.2023.11.4.1196
Iqbal, R., Ikram, N., & Shoaib, M. (2017). Phenotypic confirmatory disc diffusion test (PCDDT), double disc synergy test (DDST), E-test as diagnostic tools for detection of extended-spectrum beta-lactamase (ESBL)-producing uropathogens. Journal of Applied and Biotechnology Bioengineering, 3, 344–349. doi.org/10.15406/jabb.2017.03.00068
Issa, F. A. (2024). Antibiotic resistance patterns of common uropathogens isolated from females at Zakho City, Kurdistan Region, Iraq. Science Journal of University of Zakho, 12(4), 490–496. doi.org/10.25271/sjuoz.2024.12.4.1395
Jorgensen, J. H., McElmeel, M., Fulcher, L., & Zimmer, B. (2010). Detection of CTX-M-type extended-spectrum beta-lactamases (ESBLs) by testing with MicroScan overnight and ESBL confirmation panels. Journal of Clinical Microbiology, 48, 120–123. doi.org/10.1128/jcm.01507-09
Karigoudar, R. M., Karigoudar, M. H., Wavare, S. M., & Mangalgi, S. S. (2019). Detection of biofilm among uropathogenic Escherichia coli and its correlation with antibiotic resistance pattern. Journal of Laboratory Physicians, 11(1), 17–22. doi.org/10.4103/jlp.jlp_98_18
Kaur, J., Chopra, S., & Sheevani, G. M. (2013). Modified double disc synergy test to detect ESBL production in urinary isolates of Escherichia coli and Klebsiella pneumoniae. Journal of Clinical and Diagnostic Research, 7(2), 229–233. doi.org/10.7860/jcdr/2013/4619.2734
Liao, K., Chen, Y., Wang, M., Guo, P., Yang, Q., Ni, Y., Yu, Y., Hu, B., Sun, Z., & Huang, W. (2017). Molecular characteristics of extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae causing intra-abdominal infections from 9 tertiary hospitals in China. Diagnostic Microbiology and Infectious Disease, 87, 45–48. doi.org/10.1016/j.diagmicrobio.2016.10.007
Mackenzie, F., Miller, C., & Gould, I. M. (2002). Comparison of screening methods for TEM- and SHV-derived extended-spectrum β-lactamase detection. Clinical Microbiology and Infection, 8, 715–724. doi.org/10.1046/j.1469-0691.2002.00473.x
Manoharan, A., Premalatha, K., Chatterjee, S., Mathai, D., & SENTRY Asia Study Group. (2011). Correlation of TEM, SHV and CTX-M extended-spectrum beta-lactamases among Enterobacteriaceae with their in vitro antimicrobial susceptibility. Indian Journal of Medical Microbiology, 29(2), 161–164. doi.org/10.4103/0255-0857.81799
Michaelis, C., & Grohmann, E. (2023). Horizontal Gene Transfer of Antibiotic Resistance Genes in Biofilms. Antibiotics (Basel, Switzerland), 12(2), 328. https://doi.org/10.3390/antibiotics12020328
Monstein, H. J., Östholm‐Balkhed, Å., Nilsson, M., Nilsson, M., Dornbusch, K., & Nilsson, L. (2007). Multiplex PCR amplification assay for the detection of blaSHV, blaTEM and blaCTX‐M genes in Enterobacteriaceae. APMIS, 115, 1400–1408. doi.org/10.1111/j.1600-0463.2007.00722.x
Murray, C. J., Ikuta, K. S., Sharara, F., Swetschinski, L., Aguilar, G. R., Gray, A., ... & Johnson, S. C. (2022). Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. The Lancet, 399(10325), 629–655. doi.org/10.1016/s0140-6736(22)00947-3
Ojdana, D., Sacha, P., Wieczorek, P., Czaban, S., Michalska, A., Jaworowska, J., ... & Tryniszewska, E. (2014). The occurrence of blaCTX-M, blaSHV, and blaTEM genes in extended‐spectrum β‐lactamase‐positive strains of Klebsiella pneumoniae, Escherichia coli, and Proteus mirabilis in Poland. International Journal of Antibiotics, 2014, 935842. doi.org/10.1155/2014/935842
Oliveira, M. C., Oliveira, C. R. A., Gonçalves, K. V., Santos, M. S., Tardelli, A. C. S., & Nobre Jr, V. A. (2015). Enterobacteriaceae resistant to third-generation cephalosporins upon hospital admission: Risk factors and clinical outcomes. Brazilian Journal of Infectious Diseases, 19(3), 239–245. doi.org/10.1016/j.bjid.2015.01.006
Risal, G., Shrestha, A., Kunwar, S., Paudel, G., Dhital, R., Budha, M. B., & Nepal, R. (2018). Detection of biofilm formation by Escherichia coli with its antibiogram profile. International Journal of Community Medicine and Public Health, 5, 3771–3775. doi.org/10.18203/2394-6040.ijcmph20183562
Rupp, M. E., & Fey, P. D. (2003). Extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae: Considerations for diagnosis, prevention, and drug treatment. Drugs, 63, 353–365. doi.org/10.2165/00003495-200363040-00002
Sambrook, J., & Russell, D. (2001). Molecular cloning: A laboratory manual (3rd ed.). Cold Spring Harbor Laboratory Press. doi.org/10.1002/jobm.19840240107
Spilker, T., Coenye, T., Vandamme, P., & Lipuma, J. J. (2004). PCR-based assay for differentiation of Pseudomonas aeruginosa from other Pseudomonas species recovered from cystic fibrosis patients. Journal of Clinical Microbiology, 42, 2074–2079. doi.org/10.1128/jcm.42.5.2074-2079.2004
Stepanović, S., Vuković, D., Hola, V., Bonaventura, G. D., Djukić, S., Ćirković, I., & Ruzicka, F. (2007). Quantification of biofilm in microtiter plates: Overview of testing conditions and practical recommendations for assessment of biofilm production by Staphylococci. APMIS, 115(8), 891–899. doi.org/10.1111/j.1600-0463.2007.apm_630.x
Taher F. S. and Othman H. E. (2024). Molecular identification and genotyping of methicillin-resistant staphylococcus aureus (mrsa) in different clinical samples. Science Journal of University of Zakho. 12(2):159-68. https://DOI.org/10.25271/sjuoz.2024.12.2.1276
Tsering, D. C., Das, S., Adhikari, L., Pal, R., & Singh, T. S. (2009). Extended spectrum beta-lactamase detection in gram-negative bacilli of nosocomial origin. Journal of Global Infectious Diseases, 1(2), 87–92. doi.org/10.4103/0974-777x.56247
Turner, S., Pryer, K. M., Miao, V. P., & Palmer, J. D. (1999). Investigating deep phylogenetic relationships among cyanobacteria and plastids by small subunit rRNA sequence analysis. Journal of Eukaryotic Microbiology, 46, 327–338. doi.org/10.1111/j.1550-7408.1999.tb04612.x
Zeng, X., & Lin, J. (2013). Beta-lactamase induction and cell wall metabolism in Gram-negative bacteria. Frontiers in Microbiology, 4, 128. doi.org/10.3389/fmicb.2013.00128
Authors
Copyright (c) 2026 Alla Shamsaldin Abdullah and Pishtiwan Ahmad Hamad

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License [CC BY-NC-SA 4.0] that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work, with an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online.